It’s a story straight out of any doctor’s worst nightmare.
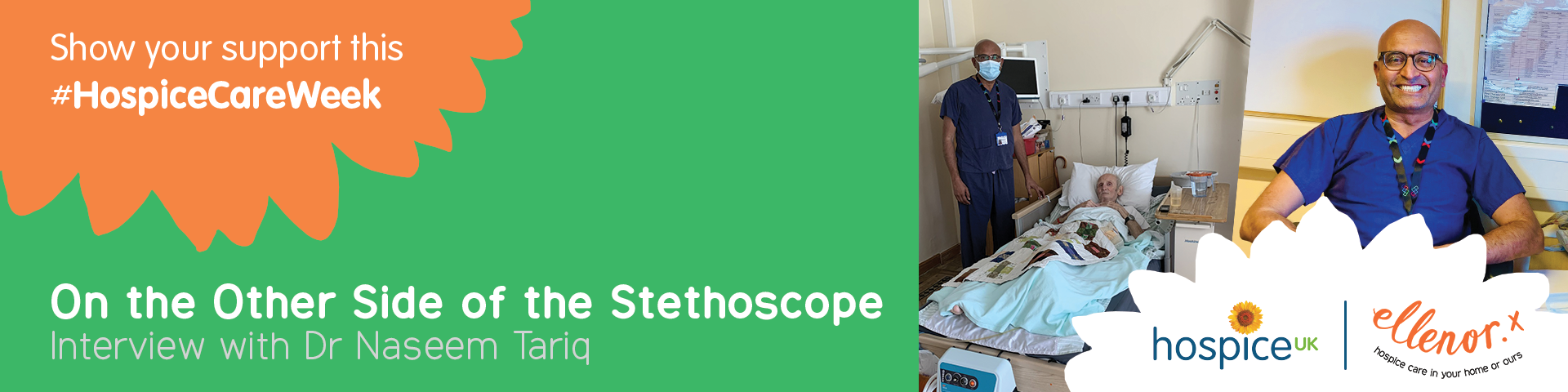
Dr Naseem Tariq was a cancer surgeon and specialist, working in acute care. Just as many of his fellow hospital-based physicians did in the early stages of 2020, during the first throes of the coronavirus pandemic, Dr Tariq caught COVID-19 himself. Unlike other colleagues who contracted COVID his condition deteriorated quickly.
Surviving COVID-19
Dr Tariq was placed on an end of life pathway, with a prognosis nothing short of devastating. In his own words, “there was no hope that I was going to survive”.
But he did. Despite declining the use of a ventilator, Dr Tariq was able to conservatively manage himself back to health, beat the virus, and survive.
Since the dawn of time, societies and cultures have placed a kind of salience on deathbed experiences – the epiphanies and realisations that emerge in the face of our potential demise. So what does a doctor – who finds himself not only on the wrong side of the stethoscope, but thrust face to face with his own mortality – learn from such a harrowing turn as a patient?
“As an end-of-life patient myself, I was felt that people never really took the time to understand what was going on with me. They asked a few standard questions, and then walked away.
"Leaving you as a patient in a very lonely place.”
With the pandemic continuing to rage, and the doctor’s perspective of acute care for End of Life fundamentally altered, Tariq became aware of ellenor through a connection with one of our staff, Dr Sheraz Majeed. ellenor is a hospice charity which cares for patients with life-limiting conditions in the Kent and Bexley localities. After Dr Tariq’s life-changing battle with illness, it was the perfect fit.
“I wanted to broaden my perspective and widen my experience, so I decided to apply to work in palliative medicine,” Dr Tariq shares. “Not working as a surgeon, but as a physician looking after patients at the end of their lives – because I have been there, and I know how lonely it is.”
Dr Tariq describes his move to ellenor as “very therapeutic” and having “offered the new perspective he was looking for”. But he’s also been able to carry over his proficiency working in an acute setting to its palliative counterpart, bringing to bear two decades of experience in a hospital to a radically different environment.
“Hospital doctors don’t know what happens to their patients when they become end of life and are transferred out of an acute setting. There’s a lot of pressure on the acute doctors, so they have no choice but to quickly turn their attention to the next patient in need of acute care. Being at ellenor now, I see that perspective – I see those patients as human beings who are no longer in the hospital, but still have a journey left in them."
"I see patients embark on a journey with us, and witness first-hand how much value we add – how much quality of life we enable them to have."
“The choices I’m able to give my patients here, I wasn’t able to provide in an acute setting because of time, acuity of patients, and different types of facilities the acute setting offers. Here, I can spend an extra half an hour with a patient. That’s what hospices can do that nobody else can. But at the same time, it’s a very different type of practice. It has a whole new impact on your personality. It changes you as a human being.”
A key tenet of ellenor’s ‘holistic’ approach to palliative care involves catering to the multiple aspects of a patient’s health. That includes treating their emotional, spiritual, social, and psychological needs, as well as their physical ones.
“What we do here is stand by our patients”, Tariq asserts. “We are there, holding their hand and being partners in their journey. We stand in for people’s fathers, mothers, grandparents, children – we are still available, even when others have left.”
The Importance of Nurses
Exemplifying the personalised, passionate approach of hospice care, Dr Tariq believes, are the efforts of ellenor’s nurses. They work both from the charity’s Northfleet-based inpatient ward, as well as providing care directly from the homes of their patients in the Gravesend community.
“No one makes this observation, but the nurses at ellenor are doing things for their patients that they probably didn’t do for their own new-born children. Here’s a dying adult, for instance, who is agitated, and totally dependent on them for personal care. The patient has wounds, they’re incontinent, they have difficulties eating.
"Nurses help them every day, and with a smile.”
Dr Tariq provides the example of one young cancer patient, who was in their late twenties when they approached the final stages of their life. “Their bravery was remarkable, but we know they were going through a bad, downhill journey in the end.
“Patients facing end-of-life face difficult situations and this can be challenging for healthcare professionals. A broad multi professional team approach, an area that hospices specialise in, is needed to support these patients and their families along their journey and the challenges they face. We managed to forge a good relationship, even with the family, and when they passed away everyone was happy that the hardship had ended in a positive way. There was closure and the family were pleased.